As we continue to become more aware of horse gut health, the topic of “hindgut ulcers” is frequently raised. The horse’s stomach can develop ulcers, so does this mean their colon can as well?
First, let’s take a look at what the hindgut is and what it does…
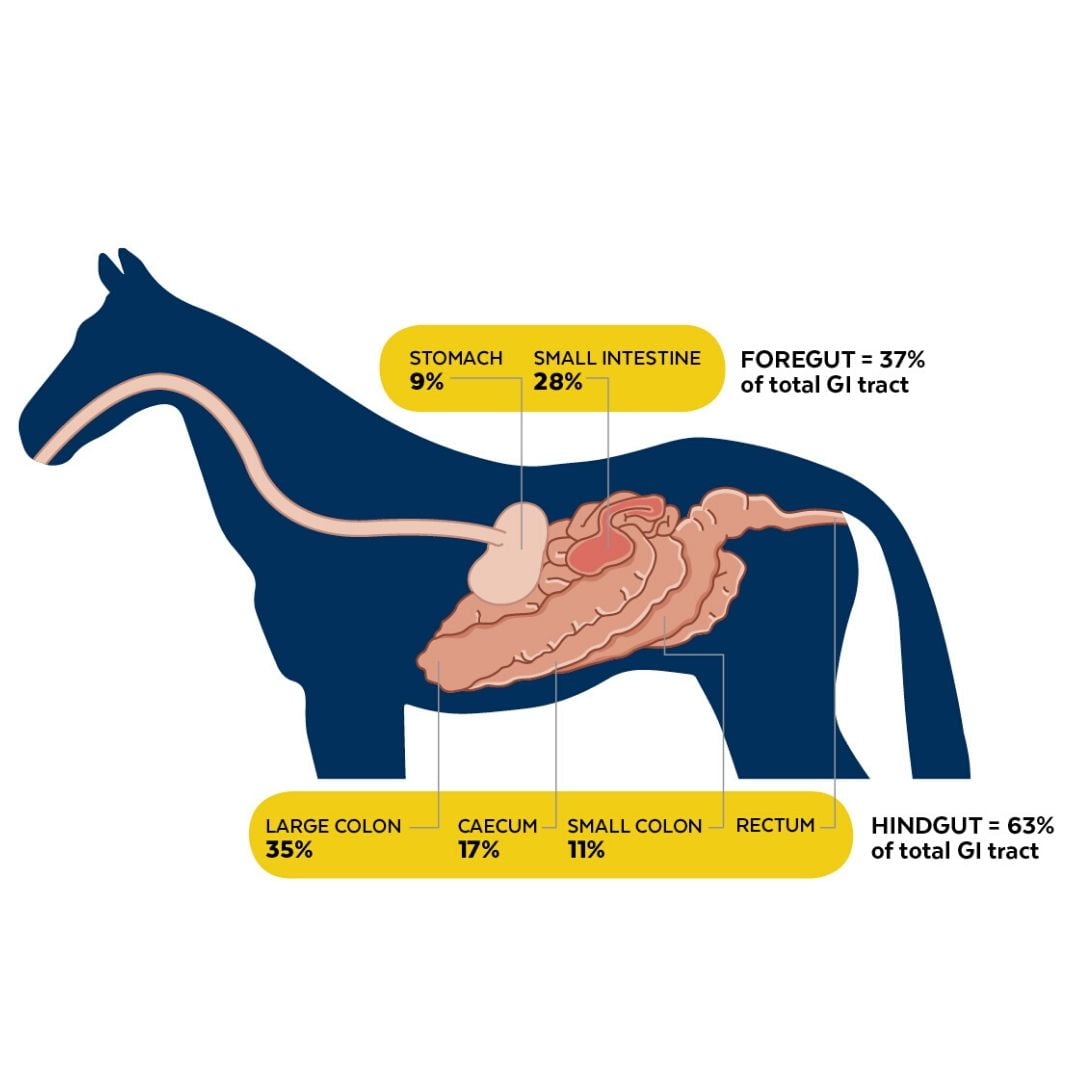
The horse’s hindgut comprises the caecum, large colon, small colon and rectum. The hindgut is the powerhouse of the horse’s digestive system and consists of 63% of the total tract. It houses trillions of microbes that produce enzymes to breakdown (ferment) plant fibre. A by-product of microbial fermentation of fibre is the production of volatile fatty acids (VFAs). VFAs provide the horse with a source of energy. In fact, approximately 70% of the horse’s energy supply comes from VFAs!
The beneficial microbes in the horse’s hindgut are in a very delicate balance and sensitive to changes in their environment. The pH of the hindgut typically rests around 6.5 – 7, which provides ideal conditions for fibre-fermenting microbes. pH is a numerical scale that tells us how acidic or alkaline a substance is. It ranges from 0 to 14, with 0 being highly acidic and 14 being highly alkaline. A pH of 7 is considered to be neutral.
Fermentation of fibre is a very slow process. Feed can take between 48 and 65 hours to travel from the end of the small intestine to the rectum, where it is expelled as manure. On the other hand, fermentation of starch and sugar is a rapid process. Problems start to occur if starch and sugar reaches the hindgut.
Hindgut acidosis is a condition that arises when undigested starch and simple sugars overflow into the hindgut where they are rapidly fermented. A by-product of this fermentation process is the production of lactic acid. This increases the acidity (decreases pH) and hence results in acidosis. As the pH drops, the fibre-fermenting bacteria begin to die off (pH<6). Conversely, lactic acid-producing bacteria proliferate in a more acidic environment. This creates a vicious cycle as the more acid these bacteria produce, the more acidic the hindgut becomes. Not good!
This leads us back to the question of hindgut ulcers…
Horses develop gastric ulcers on their stomach lining when it is repeatedly exposed to hydrochloric acid. So, it would make sense to assume that acidic conditions in the hindgut would cause ulceration on the intestinal lining. Right?
In fact, in 2005 a large-scale necropsy of 545 horses found at 44% of non-performance horses and 65% of performance horses had colonic ulcers (Pellegrini 2005)! Well, that should be pretty convincing. The problem is, this study was lacking quite a bit of information to allow for critical assessment. There is no information on the history of the horses, their diets, exposure to stressors and use of NSAIDs (e.g. phenylbutazone). It also does not distinguish between parasite lesions and other causes (such as the use of NSAIDs for right dorsal colitis).
Fast forward a decade and we have another study that showed 21% of the 56 horses had colonic ulceration (Kerbyson et al. 2017). However, 8/12 cases were due to parasite damage, 1/12 was sand ingestion, and 3/12 cases were idiopathic (i.e. cause unknown).
So, where does this leave us? As mentioned above, the only time ulcers appear in the large intestine is when they are associated with another disease process (usually parasites) or with right dorsal colitis (RDC). RDC is a term given to ulceration on the lining of upper right section of the horse’s large colon. RDC usually occurs in response to long-term, high dose treatment plans with NSAIDs (e.g. bute). In order to relieve pain, NSAIDs block the release of hormones (prostaglandins) from the damaged tissue to reduce inflammation. However, prostaglandins are also involved in blood flow regulation and mucus production in the gut. Reduced prostaglandin production therefore compromises the gut’s natural protective mechanisms.
How to diagnose hindgut ulcers?
The tricky thing about the horse’s hindgut is we are unable to scope this area to properly visualise the intestinal lining. So, how can we go about definitively diagnosing the issue?
Clinical signs of RDC include:
- Recurrent colic episodes
- Intermittent diarrhoea
- Weight loss
- Poor performance
A presumptive diagnosis of RDC can be made based on history, clinical signs and changes in blood work. Blood tests may reveal mild anaemia, increased white blood cells (WBCs), low blood proteins (albumin), high inflammatory proteins and low calcium. Perotineal (belly) fluid analysis might show a mild increase in WBC count and increase in total protein (>2.5g/dl). If the horse has diarrhoea, your veterinarian will perform faecal cultures to rule out infectious causes such as Salmonellosis and Clostridium.
Since the clinical signs for RDC are quite similar to equine gastric ulcer syndrome (EGUS), your veterinarian may put an endoscope in the horse’s stomach to rule out stomach ulcers. An abdominal ultrasound of the right dorsal colon is another diagnostic technique that may reveal thickening of the colon wall.
Treatment
Management practices include discontinuing or avoiding use of NSAIDs, reducing inflammation, frequent feedings and minimising stress (reduce strenuous exercise and travel). Feeding recommendations for horses recovering from RDC might seem counterintuitive to what we know about horse nutrition. It is important to decrease bulk in the diet to reduce mechanical load on the colon and allow it to rest. This means reducing the forage component of the horse’s diet (i.e. pasture and hay). Your vet may recommend replacing dry hay with a lucerne-based complete pelleted feed to reduce gut fill. It is important to gradually introduce the new feed over several days to allow the horse’s digestive tract to adjust to the changes. You can allow the horse to graze small amounts of fresh grass four to six times a day (10 to 15 minute intervals). The dietary change is only temporary and lasts for three to four months or when blood work returns to normal.
Medications for gastric ulcers (e.g. omeprazole, ranitidine) would not be expected to be effective in treatment of RDC. Your vet may recommend sucralfate, which is a compound that binds to the ulcer bed and forms a bandage over the ulcer. Once adhered to the ulcer, sucralfate stimulates prostaglandins, which protect the mucosal surface of the intestines.
Take Home Message
The take home message is the term “hindgut ulcers” should not be used akin to “gastric ulcers”. Gastric ulcers are wounds that develop on the stomach lining due to prolonged exposure to gastric acid. There is no acid secreting tissue past the stomach. So, “treating” your horse for hindgut ulcers is irrelevant unless they have been diagnosed with RDC.
The best way to manage hindgut health is through good nutrition, which may include a digestive health supplement, and appropriate parasite control. Use NSAIDs (e.g. bute) with caution and under veterinary advice. If you horse requires treatments with NSAIDs, a gut health supplement is recommended.
Kelato’s GastroAID Recovery and GastroAID Everyday both promote optimal stomach and hindgut health for a healthier, happier horse! If you have any questions about the best product for your horse, give us a call on 1800 KELATO or email technical@kelato.com.au!
Written for Kelato Animal Health by Natalie Hackl (BAnVetBioSc (Hons), BEqSt) – Technical Manager & Nutritionist
References
Andrews, FM, Colonic Ulcers: A Pain in the Hindgut. Equine Health Studies Program, Louisiana State University, viewed 31 October 2019, https://www.lsu.edu/vetmed/ehsp/horse_health/lsu_tips/colonic_ulcers.php
Pellegrini, FL 2005, ‘Results of a Large-Scale Necroscopic Study of Equine Colonic Ulcers’, Journal of Equine Veterinary Science, vol. 25, no. 3, pp. 113-117.
Kerbyson, NC, Knottenbelt, DC, Hotchkiss, J & Parkin, TDH 2017, ‘Idiopathic Colonic Ulceration: Prevalence, Gross Pathology and Clinical History in 56 Horses’, Equine Veterinary Journal, vol. 49, no. S51, pp. 13-16.